Cataracts are an inevitable part of aging for many, but for people living with diabetes, they often appear earlier and progress more rapidly. This acceleration is due to the long-term changes high blood sugar can trigger in the eye’s delicate lens, which can cause it to become cloudy sooner.
If you have diabetes and are considering cataract surgery, you are not alone. It is one of the most common and successful surgeries performed worldwide. However, for individuals with diabetes, achieving clear vision requires additional care and attention before and after the procedure. These extra steps are not roadblocks; they are vital precautions designed to protect your vision and ensure a smooth, safe healing process.
How Diabetes Impacts Eye Health
High blood sugar doesn’t just affect your body’s major organs; it has a profound impact on eye health.
- Accelerated Cataract Development: Chronically elevated glucose levels cause the lens to swell and then become opaque more quickly than in non-diabetic individuals.
- Increased Retinal Risk: Diabetes is the leading cause of blindness in working-age adults. It significantly increases the risk of diabetic retinopathy (damage to the retina’s blood vessels) and macular edema (swelling in the central part of the retina). These conditions, if left unmanaged, can complicate cataract surgery outcomes.
- Slowed Healing: Diabetes is known to compromise the body’s natural healing and immune response. This means wounds heal more slowly, and there is a higher, albeit still low, risk of post-operative infection or inflammation.
Because of these factors, the single most important action you can take before undergoing surgery is to achieve strict and stable blood sugar control. This proactive management is the foundation for a successful surgery and recovery.
Also Read: How Eye Doctors Detect Early Signs of Diabetes or Hypertension
Understanding Cataract Surgery
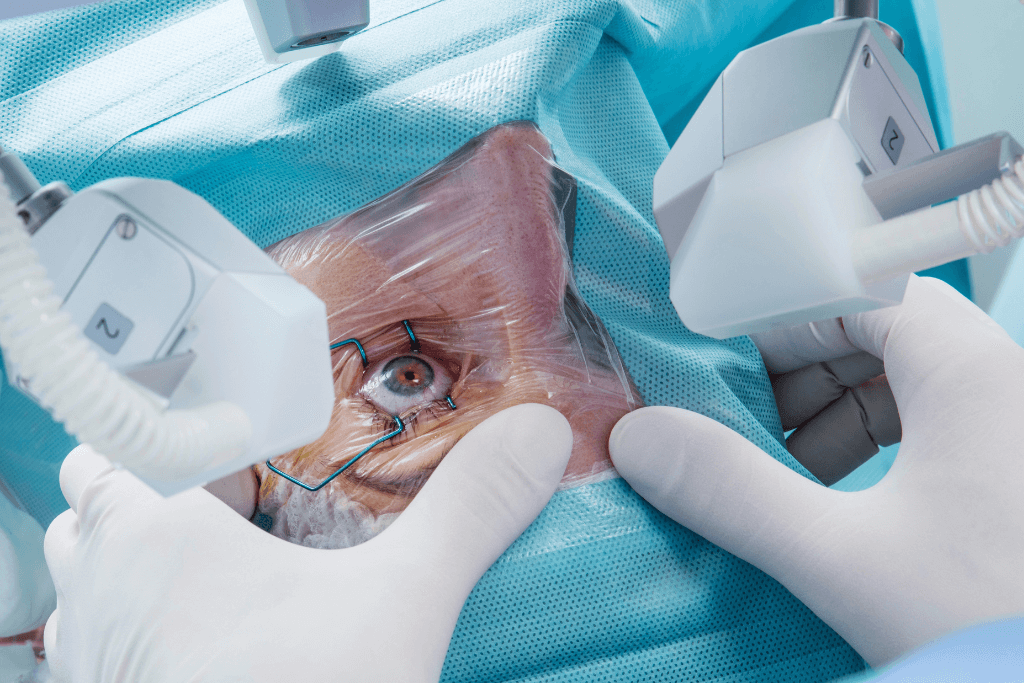
The procedure is elegant and straightforward. During cataract surgery, the surgeon makes a microscopic incision, gently breaks up the clouded natural lens (the cataract), removes it, and replaces it with a clear, artificial lens, known as an Intraocular Lens (IOL).
Cataract surgery is remarkably safe, quick, and typically performed on an outpatient basis under local anesthesia. For diabetic patients, the outcomes are generally excellent, often resulting in dramatic vision improvement, especially when all pre-operative management steps are meticulously followed.
Pre-Surgery Preparation for Diabetic Patients
A safe outcome begins long before you arrive at the surgical center. Your eye surgeon and diabetes care team must work in concert.
Medical and Blood Sugar Evaluation
It is important to have your diabetes well-controlled. Your surgeon and primary care physician will stress the importance of achieving a stable A1C (a measure of average blood sugar over two to three months) under a physician-recommended level. Surgery should generally be postponed if your A1C is significantly high or your glucose readings are volatile. Stable blood sugar reduces inflammation and enhances healing.
Retinal Examination
Before surgery, you will require a thorough retinal examination. The surgeon needs to identify any signs of pre-existing diabetic retinopathy or macular edema. If significant retinal issues are present, the surgeon may recommend treating them, often with injections or laser therapy, before cataract surgery. Addressing the retina first significantly improves overall visual outcomes after cataract removal.
Medication Adjustments
You must discuss the timing of your insulin or oral diabetes medications with your surgeon and endocrinologist. On the day of surgery, you may need to adjust your usual routine to prevent hypoglycemia (low blood sugar), as you will likely be fasting. Furthermore, certain medications, even non-diabetes-related ones like blood thinners, may need a temporary pause, so a full medication review is essential.
Post-Surgery Healing and Care
The recovery phase is where the unique challenges for diabetic patients come into play, making your discipline with post-operative instructions critical.
Immediate Post-Operative Instructions
The key to recovery is the diligent use of prescribed antibiotic and anti-inflammatory eye drops. These are your defense against infection and swelling, both of which are heightened concerns for diabetic patients. You must use them exactly as directed. Additionally, avoid eye rubbing, heavy lifting, or any activity that could put strain on the eye for the period specified by your doctor.
Blood Sugar Management
Stable glucose levels are the single most effective promoter of healing. High or wildly fluctuating blood sugar can delay recovery, increase inflammation, and raise the risk of post-operative complications, particularly the worsening of macular edema. You should monitor your glucose readings more frequently than usual in the days following surgery.
Monitoring for Complications
While complications are rare, early detection is key. You will have regular follow-up appointments to check for issues like pressure changes and the development of post-operative macular edema. You must be vigilant and report any of the following warning signs immediately: blurred vision, pain, excessive redness, or swelling that worsens rather than improves.
Long-Term Eye Health After Surgery
Cataract surgery removes one complication, but the underlying condition, diabetes, remains. Maintaining your new, clear vision relies on the ongoing, active management of your diabetes.
Regular eye exams are non-negotiable. They allow your doctor to continue monitoring for diabetic retinopathy and other changes that can occur in the retina over time. A comprehensive approach to health, including a healthy diet, consistent hydration, and rigorous blood pressure control, is necessary to support the long-term health of all the blood vessels in your eyes.
Tips for a Smoother Recovery
To set yourself up for the best possible experience, consider these practical tips:
- Timing: Plan your surgery for morning hours when your blood sugar is generally easier to manage and more stable.
- Assistance: Arrange for a friend or family member to assist with transportation and to help manage and remind you about your eye drop schedule, especially in the first few days.
- Record Keeping: Maintain a detailed written log of your blood glucose readings after surgery. Share this information with both your ophthalmologist and your diabetes care team.
- Communication: Ensure your ophthalmologist and the doctor managing your diabetes are aware of the surgical date and your recovery progress.
Also Read: Cataract Surgery 101: What Happens and How Long Recovery Takes
When to Contact Your Eye Doctor
Do not hesitate to call your eye doctor immediately if you experience any of the following:
- Sudden vision loss or a significant increase in floaters (specks or lines drifting across your vision).
- Persistent or severe eye pain, swelling, or excessive redness.
- Severe light sensitivity or any unusual discharge from the eye.
Conclusion
Cataract surgery for people with diabetes is a highly effective and safe procedure when it is supported by excellent medical control and proper follow-up. The temporary extra steps, stabilizing your blood sugar, undergoing comprehensive retinal checks, and meticulously adhering to post-operative care, are small investments that yield immense rewards: clearer, lasting vision.
Take proactive steps today by consulting with your diabetes care team and scheduling a full eye examination to discuss your options.